Q. When should you start thinking about your bone health?
A. Much earlier than you think!
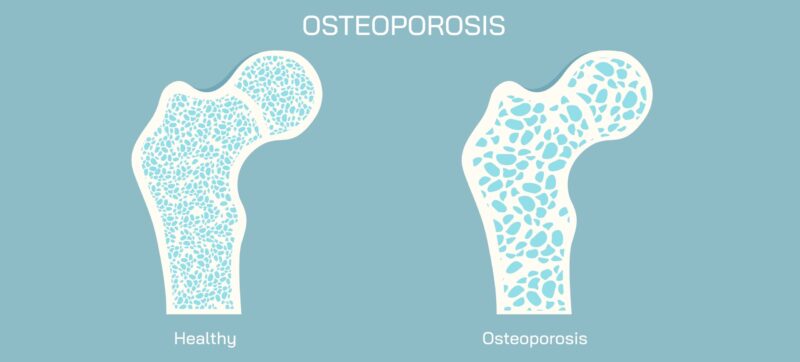
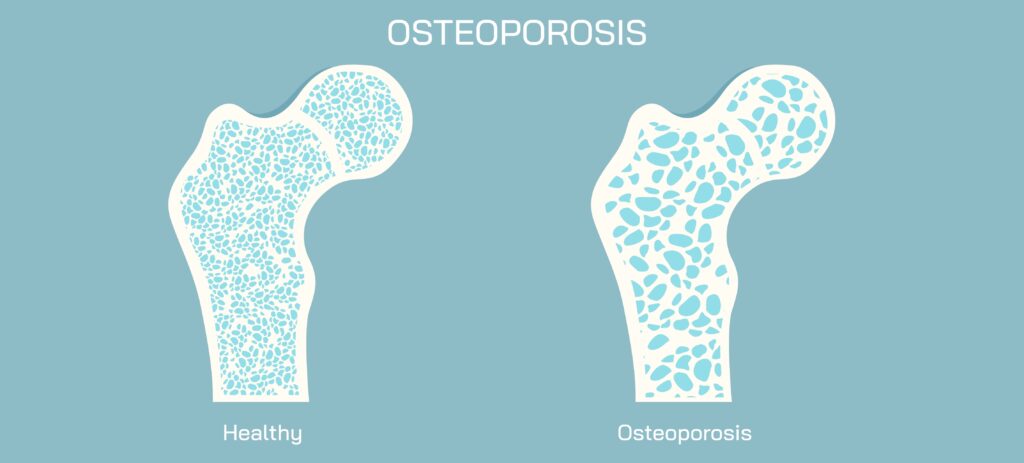
We often think of osteoporosis as something that only affects little old ladies. They shrink a bit, they start to bend over and if they fall they break bones in their arms or hip, or they fracture their spine when they sneeze or cough. These injuries can be painful and lead to a loss of independence.
The changes that make that happen in later years start decades before and accelerate around rapidly in the two years or so before menopause and the first few years after it. In fact, according to Dr Mike McClung, endocrinologist and world authority on bone health who was instrumental in working with the World Health Organisation on developing the fracture risk scores we use today, we lost around 18-20% of bone mineral density – the stuff that makes our bones strong and resistance to fractures – around that menopause transition. And he says, if you enter that phase of your life with an already low-ish bone mineral density, the chances are very high that you’ll have osteoporosis in your mid 60’s. In fact, the Endocrine Society says 1 in 10 women over the age of 60 have osteoporosis.[1]
How does this happen?
First up, let’s take a little look at bones. They aren’t static structures, they’re constantly remodelling – breaking up and building down all the time and it’s said that we replace our entire skeleton every decade. Osteoclast and osteoblast are the drivers behind this. The osteoclasts break bone down and the osteoblasts build it back. Osteoclasts activity is controlled by oestrogen, so when we go through menopause and those levels are simultaneously fluctuating and declining, it plays havoc with that regulatory system. Over time the body adapts and that resorption of bones continues to decline, but not as rapidly.
How do we know it’s happening?
Bone loss is, unfortunately silent – we have no idea that it’s going on. Being bone female is a risk factor but there are others too, so if you have any of these speak to your doctor about organising a scan.
- Low BMI – low or underweight people are at greater risk
- A family history of osteoporosis, or is you’re unsure, have any of your relatives had broken hips or broken arms as they’ve aged after a fall from a standing height, or spinal fractures
- A history of having no periods (apart from pregnancy)
- A history of using high strength cortocosteriods
- Are a smoker.
The only way to tell what our bone density is, is to have a scan, often referred to as a DEXA scan. It uses low dose radiation to see how dense or strong the bones. This density if rates giving you a ‘T score’ which is a comparison of your bones density to what you’d find in healthy, younger adults. Peak bone density occurs once we stop growing, so early late teens/early adulthood, which is why that’s the comparison group, the aim being to find out how far you are from what was the norm around peak bone strength.
The T score scales are:
- Normal (+1 to -1) – Your bone density is in the normal range
- Low bone density (-1 to -2.5) – Your bone density is slightly below the normal range and is considered to be the range that would be considered as osteopenia range. This score is common in older adults, with around 54% of women falling into this category.[2] Osteopenia is a condition where bone mineral density is lower than average but not low enough to be considered osteoporosis. It’s important to remember though that not everyone who has osteopenia will progress to osteoporosis.
- Osteoporosis (-2.5 and below) – Your bone density is much lower than the normal range for a young adult. This is also known as the osteoporosis range.
You may also be given a Z score, which compares you to the average of people around your own age – which as we’ve seen, is more likely than not, to be suboptimal.
Dr McClung says, if we’re in heading into menopause it’s probably a good idea to get one of these scans, because if you’re about to start that rapid phase of bone loss and you already have a lower than normal bone density, that loss of 20% means you could be osteoporotic a good 15-20 years before someone with ‘normal’ bone density. But, there are things that can help.

Are Lifestyle Measures Enough?
Diet, vitamin D, calcium, and resistance training are widely promoted for bone health—and rightly so. These lifestyle factors are critical, especially in childhood and adolescence when peak bone mass is being built. However, during the menopausal transition when oestrogen levels drop, Dr McClung says they’re important, but “they are not sufficient. Weight bearing exercise is really important in kids, while they’re growing to improve and optimize their peak bone mass, and it’s important in elderly people to be remain physically active, that can slow the age related loss of bone density, but the rapid loss happens across the menopausal transition is clearly related to oestrogen deficiency, and none of the general measures are effective in preventing that from happening.”
Studies comparing women who did a lot of weight bearing exercise to those who did not found there was only about a 2% advantage in the exercise group. “So, while it’s important to do those things for women who come to menopause with low or low normal bone density, something more should be considered to protect them from developing osteoporosis.”
What do we do?
The first line treatment he says is oestrogen, according to Dr McClung. If you are unable to take HRT then there are other medications, commonly called bisphosphonates that can provide protection during this phase of rapid loss too.
While it is important to do weight bearing exercise, not smoke, get enough calcium in your diet (around 1200mg/day) as well as adequate vitamin D intake, other interventions should be considered.
According to Dr McClung the optimal oestrogen dosing is:
- Oral estradiol: 1 mg/day
- Transdermal estradiol: 0.1 mg/day
In terms of serum levels, he says during that phase you should be looking at around 40 picograms per milliliter (pg/mL). In the UK that equates to around 140 pmol/L.
After the rapid-loss phase, doses can often be halved for long-term maintenance.
Alternatives to oestrogen
- For women who cannot take oestrogen or do not wish to bisphosphonates are effective:
- Alendronate: 35 mg/week for prevention
- Zoledronate: Single IV dose every 2 years for prevention or every 5 years for maintenance
- Raloxifene has only weak effects and is generally not effective around menopause.
What About Other Hormones?
Progesterone has no direct impact on bone, McClung says. Some synthetic progestins may offer minor benefits due to their androgenic effects, but they are not considered reliable options for bone protection.
Testosterone is often touted for muscle mass preservation and bone strength. However, its bone benefits are largely due to its conversion to oestrogen. Even in men, testosterone supplementation shows limited efficacy in improving bone health unless it converts to oestrogen. In postmenopausal women, there is not enough evidence to recommend testosterone for osteoporosis prevention.
Lifelong Bone Health Strategy
It’s never too late to take care of your bones – and it’s never too early.
Dr McClung says we need to adopt a life-long approach to bone health. If you have children, running, skipping and any exercise that puts force through the bones can help them ensure they have good strong bones when the reach adulthood. He recommends:
- Childhood & adolescence: Optimize peak bone mass through physical activity and good nutrition.
- 20s–40s: Avoid harmful habits (smoking, excessive alcohol), if you are regularly missing periods get it checked.
- Menopause transition: Consider oestrogen or bisphosphonates based on risk.
- Post-menopause (maintenance): either stay on oestrogen at a lower dose or consider intermittent therapy (e.g., zoledronate every 5 years) can preserve bone density safely and effectively for life.
- Do keep moving – weight bearing exercise throughout life is a must do – walking, running, lifting weights. And, don’t forget your balance – you’re less likely to fall if you have good balance – and if you don’t fall, you’re less likely to break a bone in the first place.
You can watch the interview with Dr Mike McClung here.
[1] https://www.endocrine.org/patient-engagement/endocrine-library/menopause-and-bone-loss